Occupational Therapy (Adults)
Occupational Therapy is a health profession that helps people of all ages lead a more productive, satisfying and independent life. Fundamental to the practice of Occupational Therapy is the person’s occupations which are defined as the tasks and activities that occupy a person’s time and energy throughout the day. This can include things like getting dressed, preparing a meal, working at a job, playing, attending school, and enjoying time with family or friends. Occupational Therapy helps individuals to perform the occupations they need to and want to do.
Working as part of the health-care team, the occupational therapist (OT) considers the client’s occupations, abilities (physical, affective, and cognitive), their environment and their specific needs and goals. An OT is an expert at analyzing the effects of the client’s environment and functional limitations on their ability to perform their day-to-day tasks and activities. Once an assessment has been completed, the OT works with the client to help him/her fulfill roles as a parent, child, spouse, student, worker, or team player.
Acute care inpatient services
Working collaboratively as part of the patient care unit teams, OTs are one of several disciplines assisting patients and families to successfully transition to the community as independently as possible. OTs also work closely with Rehabilitation Assistants and other support staff to support inpatient care.
Acute care services provided by OTs include:
- Assessment of the patient’s self-care and home management activity skills related to acquired, developmental, chronic or acute conditions
- Assessment of the patient’s physical, cognitive, perceptual-motor, socio-cultural and emotional capabilities related to their self-care and home management activities and routines
- In-hospital assessments of physical, social, and cultural environments
- Discharge planning/risk assessment
- Equipment and assistive devices prescription
- 24-hour pressure management
- Acute wheelchair mobility, and seating/positioning assessments and intervention
- Post-surgical or post-trauma wound care, splinting, casting and associated interventions
- Scar management and burn scar pressure garment intervention
- Referral to community support services
Acute care areas served
- Medicine Units
- Surgery Units
- Emergency and Observation
- Women’s Health Units
- Transplants
- Inpatient Burns & Plastics
- Clinical Assessment Unit
- Intermediate Intensive Care Unit
- Medical Intensive Care Unit
- Surgical Intensive Care Unit
Working together with families
Patients often come with a team of people important to them who have been and will continue to support them in their life journey. We consider these people part of our care team as well and may include them in assessment, interventions and planning.
There are times when OT staff may reach out to family members or other caregivers to assist us to meet the care needs of our patients. We will always have patient permission to make this contact for all competent patients.
We may make contact to help us with collateral information or to understand information regarding assistance being received in the home environment and/or equipment or adaptations in place. Sometimes we need assistance obtaining very specific information, such as pictures or measurements from the home environment that will help us in the planning we are doing with the patient. We may also request assistance with bringing in the patient’s clothing, toiletries or existing equipment to assist in our assessment and interventions.
At times, we may request a meeting with family or other caregivers to come on-site and learn something new related to caring for the patient, assist with the training for using equipment that may be required, or be part of the assessment and discussions.
Contact information
700 William Avenue
Monday – Friday: 7:45 a.m. – 4 p.m.
Saturday/statutory holidays: 7:30 a.m. – 15:45 p.m. only for discharge planning services for clients in Adult Acute Care
Rehabilitation Inpatient Services
Working collaboratively as part of the RR5 patient care unit team, Occupational Therapists (OT) are one of several rehabilitation professionals assisting patients and families to set and meet their goals to successfully transition to the community as independently as possible. OTs also work closely with Rehabilitation Assistants and other support staff to support inpatient care.
Rehabilitation services providing by OTs include:
- Rehabilitation, habilitation, or maintenance of the client’s self-care, mobility and home management activity skills related to acquired, developmental, chronic or acute conditions
- Assessment of the client’s physical, cognitive, perceptual-motor, socio-cultural and emotional capabilities related to their self-care, mobility and home management routines
- In-hospital &/or community-based assessments of physical, social, & cultural environments
- Interventions to maximize independence in everyday tasks through remedial and/or compensatory methods
- Upper extremity assessment and interventions (i.e. splinting)
- Discharge planning/risk assessment
- Equipment & assistive devices prescription
- Assessment & training in commercial or customized assistive technologies (i.e. computer access systems and environmental controls)
- 24-hour pressure management
- Wheelchair mobility & seating/positioning assessments & intervention
- Training for patient self-management and direction of their care in the community
- Orientation & referral to community support services
Working with families and Essential Care Partners
Patients often come with a team of people important to them who have been and will continue to support them in their life journey. We consider these people part of our care team as well and may include them in assessment, interventions and planning.
There are times when OT staff may reach out to family members or essential care partners, other caregivers, etc. to assist us to meet the care needs of our patients. We will always have patient permission to make this contact for all competent patients.
We may make contact to help us with collateral information or to understand information regarding assistance being received in the home environment and/or equipment or adaptations in place, etc. Sometimes we are wanting assistance obtaining very specific information such as pictures or measurements from the home environment that will help us in the planning we are doing with the patient. We may also request assistance with bringing in the patient’s clothing, toiletries or existing equipment to assist in our assessment and interventions.
At times we may be requesting a meeting with family or other caregivers to come on site and learn something new related to caring for the patient, assist with the training for using equipment that may be required, be part of the assessment and discussions, etc.
Rehabilitation populations served
- Spinal Cord Injury
- Amputations
- Neuromusculoskeletal
Contact information
Monday – Friday: 8 a.m. – 4:15 p.m.
800 Sherbrook Street
Winnipeg, Manitoba
Resources
Outpatient care
Adult (Upper Extremity) Hands Rehabilitation Service
The Adult (Upper Extremity) Hands Rehabilitation outpatient service is a comprehensive, collaborative, and client-centred service providing assessment and intervention for individuals with a surgical or traumatic upper extremity condition. The Occupational Therapists (OT) working in this service specialize in the fabrication and provision of custom orthoses/splints for protection post-surgery, to prevent deformity, for exercise to restore joint mobility, and/or to enhance function in daily activities. OTs collaborate with clients to establish treatment goals and communicate with the surgeons and physiotherapists on a cross-referral basis to help further improve upper extremity mobility, strength, and/or function.
Services provided
Comprehensive assessment and treatment of the upper extremities, including:
- Education regarding injury, surgery (if applicable), and rehabilitation process
- Surgical wound care assessment
- Edema (swelling) assessment and management
- Scar assessment and management
- Sensory assessment and management
- Range of motion assessment with a guided exercise program
- Strength assessment with a guided exercise program
- Custom splinting
- Functional adaptations –assistive devices/equipment
- Nerve recovery
- Neuromuscular electrical stimulation (NMES)
- Client advocacy
- Referral to other professionals/services as determined
Criteria for referrals
Referrals are accepted for youth 16+ and adults living within the Winnipeg Regional Health Authority and the Interlake-Eastern Health Authority region (subject to change), requiring occupational therapy assessment and intervention for surgical or traumatic injuries to the digits, hand, wrist and elbow.
Referrals must be initiated from a medical doctor or a physiotherapist who is providing treatment for that injury.
Referral process
Our referral sources are primarily from Plastic and Orthopedic surgeons but referrals are accepted from family practitioners and may be considered from other allied health professionals. All referrals can be faxed to 204-787-1101.
Referral information should include:
- Diagnosis
- Injury/surgery date
- Presenting issues
- Examples: limited active range of motion (AROM), limited passive range of motion (PROM), splinting needs
- Accommodations required: language interpreter, wheelchair dependent/limited mobility, decreased cognition (issues with memory, comprehension) requiring a companion to appointments.
All submitted referrals are screened within one to two business days of receipt of referral and are scheduled based on priority/urgency. Typically, urgent referrals are seen within 1-5 days post-operative. Non-urgent referrals may be seen within 2-4 weeks of receipt of the referral. These timelines may vary depending on referrals volumes and additional details specific to each referral.
When to send a referral
Referrals need to be sent as soon as possible. Delays in initiating a referral could negatively impact an individual’s recovery. Post-op referrals should be faxed to our department the same day as surgery, especially if splinting is requested 3-5 days after surgery. Pre-operative referrals are accepted as well.
Our service routinely books clients 3-5 days post op or post traumatic injury and this is based on surgeon’s preference.
For referrals requiring splinting to recover movement in stiff joints: this can typically begin as soon as your doctor allows stretching and loading through that joint. These splints are most effective when used as early as possible in your recovery and/or when used in conjunction with other treatments such as Physiotherapy.
Header text
What to expect
- Intake and booking your first appointment
- Once your referral is received and screened, office staff will call you to schedule an initial appointment. Information provided will include purpose of your referral, our location within the hospital, and the length of your appointment. Typically, an initial appointment is 60-90 minutes in duration.
- On the day of your appointment:
- Please enter the OT Department and proceed to the office to check in for your appointment and to present your Manitoba Health card.
- Your OT will provide a comprehensive assessment and will recommend treatment of your upper extremity tailored to the diagnosis on the referral. The duration of OT intervention required and expectations will be shared. Your preferences and willingness to pursue the recommended interventions will be discussed. Your outcomes will depend on many factors, including your follow through with a home program
- You may be in a bulky dressing or a temporary cast that your doctor has asked us to remove. We will provide wound care, apply a new dressing, and provide you with an appropriate splint and range of motion exercises.
- Follow-up appointments:
- Your OT will determine a plan with you for follow-up appointments and interventions based on your initial assessment findings.
- Follow-up appointments can be in person or virtual (Microsoft Teams or phone) depending on your needs and what is most appropriate for your care.
- Appointments are often 30-60 minutes in duration and can be as frequent as 1-2 appointments per week or every 2 weeks depending on your care needs.
Treatment may be ongoing for 10-12 weeks or longer depending on the complexity of the injury or condition. Follow-up appointments could involve dressing changes, reassessment of range of motion/strength, changes to home exercise programs, and/or splint adjustments. We routinely communicate your progress to other team members such as your surgeon/physiotherapy.
Regular attendance at scheduled appointments and follow through with treatment recommended and home activities is expected and will assist your recovery. Attendance policies are in place and discharge from the service may occur for non-attendance or inconsistent attendance that is negatively impacting your outcomes.
Contact information
Monday – Friday: 8:00 am -4:00pm
Location: Rehab/Respiratory Hospital, RR180, OT Department Pink Goose Level 1
Mail: RR180-820 Sherbrook Street
Winnipeg, MB Canada R3A 1R9
Phone: (204) 787-2786
Fax: (204)787-1101
Assistive Technology (AT)
The Occupational Therapists (OT) working in the Assistive Technology program are available to assist individuals who are experiencing challenges operating technology devices (computer and/or phones), driving a power wheelchair, and/or controlling critical aspects of their home environment.
Referrals for AT OT services are accepted from an individual’s primary therapist as this service operates consultatively.
Criteria for referrals
Referral requirements for this service include the following:
- Individuals who are 18 years or older
- Referred individuals have a condition that impacts their abilities to use technology, operate a power wheelchair or control home environment
- Must have a primary therapist who agrees to remain actively involved throughout the consultative process
How to submit a referral
Therapist must complete the ATPS referral form indicating the services required and fax the completed referral to 204-787-5099.
What to expect
All new OT referrals to the AT program are screened within one week of receiving them. OT services will contact the client or referral source to schedule an initial assessment, usually within 4-6 weeks of referral being received.
Initial assessments typically take 1-2 hours and are regularly completed virtually using Microsoft Teams to provide the AT OT an opportunity to confirm the client’s goals and barriers. Clients will often also require an in-person follow-up and trial appointment which take place at our AT clinic located at 59 Pearl Street, Level 0 of the HSC Material Handlings Building.
Clients have the opportunity throughout the assessment process to trial equipment during appointments and potentially receive loan AT equipment for up to 3 weeks to trial more extensively in other environments. Clients are encouraged to have family and community support systems involved and attend appointments during the AT assessment process to assist with learning new technology solutions.
AT equipment recommendations are provided to client and primary therapist to pursue purchasing. AT OT can assist as needed with navigating funding agencies, providing justification and liaise with AT mechanical and electronic services if custom solutions or modifications to commercial equipment are required.
Contact information
Mailing address:
Health Sciences Centre Winnipeg
MH036 – 59 Pearl Street
Winnipeg, MB R3E 3L7
Assistive Technology OT Clinical Service Leader:
- Phone: 204-787-2370
- Fax: 204-787-5099
Driving Assessment and Management Program (DAMP)
The Health Sciences Centre Occupational Therapy Department Driver Assessment & Management Program (DAMP) is a comprehensive program that evaluates the needs and the potential of drivers identified as having a medically-related issue which may impact the ability to drive safely. The assessment consists of an interview, a clinical pre-screening session, a practical on-road evaluation, and a feedback session.
DAMP referral process
Driving safely requires excellent physical, cognitive, and visual-perceptual skills, as well as quick awareness, information processing, and good judgment. Physicians and Optometrists have a legal and legislated responsibility to forward medical information related to driving safety to Manitoba Public Insurance (MPI) Driver Fitness. New drivers also have a responsibility to disclose medical related information prior to applying for a driver’s licence, and experienced drivers have a responsibility to report any medical changes which may have an impact on driving ability.
Driving safely requires excellent physical, cognitive, and visual-perceptual skills, as well as quick awareness, information processing, and good judgment. Physicians and Optometrists have a legal and legislated responsibility to forward medical information related to driving safety to Manitoba Public Insurance (MPI) Driver Fitness. New drivers also have a responsibility to disclose medical related information prior to applying for a driver’s licence, and experienced drivers have a responsibility to report any medical changes which may have an impact on driving ability.
Driving safely requires excellent physical, cognitive, and visual-perceptual skills, as well as quick awareness, information processing, and good judgment. Physicians and Optometrists have a legal and legislated responsibility to forward medical information related to driving safety to Manitoba Public Insurance (MPI) Driver Fitness. New drivers also have a responsibility to disclose medical related information prior to applying for a driver’s licence, and experienced drivers have a responsibility to report any medical changes which may have an impact on driving ability.
MPI Driver Fitness refers directly to DAMP after considering all of the information provided by physicians, optometrist and drivers.
MPI website links for health-care professionals:
Preparing for a DAMP appointment
Once a referral is received from MPI Driver Fitness and we are ready to book your appointment, the OT Department will mail you a letter which describes the program, the DAMP process, and tells you how to set up an appointment.
Prior to attending your DAMP appointment, there may be some things you can do to help prepare yourself:
- If you have a valid licence, consider taking a brush-up driving lesson to refresh your driving skills, and update your knowledge of newer driving rules and regulations.
- If you do not have a valid licence, it can be beneficial to practice making driving observations and decisions while travelling as a passenger.
- You may find it helpful to refresh and update your driving knowledge. Although this is not the focus of the DAMP assessment, bad habits and rusty driving knowledge can lead to questions regarding overall driving potential and ability.
- You may anticipate the need for vehicle modifications and can review some Vehicle Modification Resources to familiarize yourself with some potential options.
During our assessment, we look at your general abilities such as your strength, range of motion, coordination, thinking speed, and ability to pay attention. These assessments are not something you can practice or study for.
What to bring
- Driving Instructor fee in cash (as per the letter you will receive).
- Driving is considered a privilege and, therefore, most medical assessments related to driving are not covered by the Canadian health care system. Fortunately, Manitoba Health does cover the clinical assessment involving the DAMP OT and the OT portion of the on-road assessment.
- The driving instructor is an independent contractor to our program and their portion of the on-road assessment is not covered by Manitoba Health. The fee covers the cost of the driving instructor and the use of their vehicle for the on-road portion.
- Reading glasses, driving glasses, sunglasses (if needed), driver’s licence (if valid)
- If English is not your primary language and you wish to have a qualified interpreter assist with communication, interpreter services can be provided in many languages at no cost to you. Please inform the receptionist when you call to book your appointment.
What to expect during your appointment
Session 1: Virtual Interview
A 30-60 minute virtual interview/assessment will be conducted in your own home using the internet and a computer, or a phone or tablet. Here, you will be asked questions about your driving history and experience, your medical history and current medical status, as well as your goals for driving. Information regarding the upcoming in-person DAMP assessment will also be reviewed and any questions you may have can be addressed during this time. If you wish, a family member, spouse, or close support person may participate in this session. If they do not live with you, we can make arrangements to include them virtually.
Session 2: In-Clinic Assessment
This portion of the assessment is conducted in the Occupational Therapy Department for 30-60 minutes where you will be asked to complete a series of tests.
Driving is a complex task that involves many different skills. This preliminary assessment provides information regarding the skills required for driving and the need for vehicle modifications.
Here, your physical function (strength, range of motion, coordination, endurance, sensation, etc.), visual-perceptual function (neglect, spatial relations, figure ground, visual discrimination, visual scanning, etc.), cognitive function (memory, attention, processing speed, judgment, road sign recognition, etc.), stationary vehicle access and control, gas/brake reaction time, and specific driving needs will be assessed.
Following the in-clinic assessment, most clients will be evaluated on the road. However, clients who cannot transfer into a driver’s seat and clients with no prior driving experience are not routinely evaluated on the road. Decisions and initial recommendations are made based on the in-clinic assessment, and further assessment may be required.
Session 3: On-Road Evaluation
If the Occupational Therapist determines that the client meets the minimal requirements for operation of a motor vehicle, an on-road evaluation is conducted immediately following the pre-screening. The approximately 45 minute in-car evaluation is done in Winnipeg only, in a dual-controlled vehicle, with the Driving Instructor affiliated with the program and the Occupational Therapist. The client’s judgment, concentration, and physical management of the car is observed in a variety of driving situations. The use of adaptive controls such as spinner devices, left foot gas pedal or hand controls is assessed as required.
Our job is not to ‘pass’ or ‘fail’ people based on their mistakes. The goal of the assessment is to determine if your medical condition is impacting your ability to drive safely. If it is, there may be recommendations we can make to help you continue or return to driving.
The majority of people we see have had a break from driving ranging from several months to several years. We understand that there will be a certain level of stress and “feeling rusty”. If you do not live or commonly drive in Winnipeg, the differences between rural and urban driving are identified and we recognize that driving in unfamiliar areas adds stress. We focus on the basic skills that every driver must have if they hold a driver’s licence, no matter where they live and drive.
Every attempt is made to position you as comfortably as possible. We can add cushions and back support if needed and assist you with getting in and out of the vehicle. The drive is about 45 minutes long, which gives most people time to adjust to the vehicle. We recognize that you will not be as comfortable as you would be in your own vehicle. If your ability to get in and out of a small SUV is a significant concern for you or you receive specific assistance from a significant other or family member, please contact the DAMP office.
The on-road portion of the assessment is not an MPI driver’s test and driver’s licences are not issued or suspended on the day of assessment.
Session 4: Feedback
Time permitting, a brief feedback session will be conducted immediately following the on-road evaluation, where the results of your assessment will be discussed. If there is detailed information and recommendations to review, a feedback session may be scheduled with you to happen virtually, by phone or video, on a different day. You may choose to invite a family member or spouse to join this session, if conducted virtually.
What to expect after your appointment
Performance on the in-clinic and on-road evaluations is summarized by the Occupational Therapist. A report detailing the client’s abilities, areas of concerns, and recommendations is sent to Manitoba Public Insurance Driver Fitness, the referring physician, and the client’s Health Sciences Centre medical record.
Recommendations may include:
- A need for further assessment
- Training with a driving instructor
- Vehicle modifications (a copy of the recommendation section of the report will be mailed to the client)
- Licence restrictions
- Resume driving without restrictions
- Driving retirement
Once your report has been reviewed by MPI Driver Fitness, they will send you a letter informing you how to proceed. MPI makes the final decision on all licensing matters. A follow-up on-road evaluation with an MPI examiner is commonly requested prior to issuing a full driver’s licence.
Planning ahead – Resources for older drivers
Our primary goal is to try to find ways to assist clients to continue or resume driving. Strategies such as ways to compensate for identified changes, vehicle adaptations, refresher courses and on-road driving lessons will be considered for each client. However, sometimes the safest recommendation is to retire or discontinue driving. This recommendation can have a significant impact on people’s lives, but there are ways to plan ahead and ease this transition.
- Keep your driving skills updated and make informed decisions about continuing to drive:
- Explore alternative transportation options:
- Winnipeg Transit Plus information and application
- TONS Quick Reference Transportation List
- Reach out to family and friends who may be able to provide transportation assistance
- Explore local meal delivery and grocery delivery services in your area
- It may be necessary to consider relocating to an area with more community resources if options are limited where you live now.
Vehicle modification resources
Vehicle control modifications for steering, gas/brake access, and secondary function access, including the washer/wipers, dimmer, and turn signal must be listed as restrictions on a valid licence prior to having them installed in your vehicle. There are many commercially available driving modifications and vehicle accessibility products that can be purchased through various medical supply stores and private vendors. Vehicle modifications must be provided by a certified installer. An occupational therapy consultation is recommended prior to equipment order and installation.
Commercially Available Vehicle Modifications
- National Mobility Equipment Dealers Association (NMEDA)
- Association for Driver Rehabilitation Specialists (ADED) – Customer Solutions
- Sure Grip adaptive equipment
- Mobility Innovations / Veigel adaptive equipment
- Adapt solutions equipment
- BraunAbility vehicles and adaptive equipment
- Vantage Mobility van conversions
- Winnipeg vendor list
- Rural Manitoba vendor list
Custom-Made Vehicle Modifications
Drivers who require vehicle modifications, and for whom commercially available vehicle modifications are not suitable, may be eligible for specialized vehicle modification services, through the Health Sciences Centre Assistive Technology Products and Services (ATPS).
You must be evaluated by the DAMP OT to determine if commercially available vehicle modifications will be suitable for you, or if specialized modifications are necessary. If custom modifications are required, the DAMP OT will coordinate a referral to ATPS.
Process for past customers of ATPS who require modifications in a new vehicle
ATPS was previously known as Rehab Engineering, and due to many changes in the program and increased availability of commercial products from vendors, some custom modifications are no longer available. Drivers who have not experienced a medical change, but require modifications in a new vehicle and have not recently been through ATPS, will need to be reviewed by the AT Intake Team. Consultation with the DAMP OT may be required to assist in determining if custom or commercial modifications are recommended. Through this process, the DAMP OT may need to communicate with MPI to notify them of updates or changes to the licence addendum or to report any major changes. When you come for your appointment, we ask that you sign a consent form that allows OT to communicate with MPI, as needed. ATPS charges for specialized vehicle modifications and once an assessment is completed, a written quote will be provided prior to the start of any jobs. For further information, please contact:
ATPS Coordinator
Assistive Technology Products and Services (ATPS)
59 Pearl Street, Winnipeg
204-787-2370
Please note, the Left Foot Accelerator is no longer available through ATPS and can be purchased through a private vendor.
Funding sources
Vehicle adaptations and modifications can be expensive, but there may be ways to obtain funding or financial assistance. The DAMP OT can provide a copy of your DAMP report if needed when applying for funding.
- Labatt Better Together
- I Am Ministries and Keith Howell Mobility Trust
- MS Society – Quality of Life grant
- Manitoba Possible Vocational Rehabilitation
- Spinal Cord Injury Manitoba
- The Manitoba Paraplegic Foundation
- War Amps
Driving Lessons
Once you have received a valid licence listing the required driving modifications, you may pursue having your own vehicle modified. If you wish to take driving lessons, you may contact any driving instructor to request lessons in your own modified vehicle. A temporary instructor brake is typically required for this option. Alternately, you may contact the Rehab Driving Instructor for lessons using the instructor’s vehicle with the appropriate modifications. Please use your copy of the DAMP recommendations as reference for specific equipment information.
- Metro Driving School – Mit Kinnarath
- Phone: 204-955-1440
- Email: [email protected]
Multiple Sclerosis Service
The adult multiple sclerosis outpatient occupational therapy (OT) service focus is on assessment and intervention for clients with issues relating to multiple sclerosis and allied conditions symptoms and functional challenges related to episodic issues or progressive disease.
Referral criteria
- Must have a multiple sclerosis or allied conditions diagnosis
- Referrals must be made by physicians but may be accepted from other allied health professionals on a case-by-case basis
- Client is 16+ years old
Services provided
- Initial assessment for client and therapist to meet and discuss current issues relating to their diagnosis and participation in daily activities
- Education regarding health condition(s)
- Client-centered collaboration to help maximize meaningful occupations
- Custom orthoses/splinting for pain control and/or joint positioning
- Seating and positioning
- Pressure management
- Review and recommendation of assistive devices and equipment
- Cognition and executive function assessment and intervention
- Fatigue management/sensory processing assessment and intervention
- Client advocacy
- Referral to other community supports as determined
Referral process
Once a referral is received, it is screened by the occupational therapist to ensure the client is eligible for the services. The referral is placed on the waitlist. Once the client can be scheduled, the client is contacted by the office staff of the OT Department, typically by telephone, to book an initial appointment which may be on the phone, by video, or in person at our site. Please fax all referrals to 204-787-1101.
What to expect
The initial appointment with the occupational therapist can typically be 60-90 minutes in length for assessment and intervention of presenting issues. When you arrive, please check-in for your appointment at our main office. The occupational therapist will review the referral information, discuss available options for intervention and provide those during the appointment after a plan is agreed upon with the client. Follow-ups may be scheduled depending on need. Follow-ups may be conducted virtually or in-person.
How to find us
The multiple sclerosis occupational therapy service is located at RR-180, 800 Sherbrook Street, Pink Goose Zone, Level 1.
Phone Number: 204-787-2786
Fax Number: 204-787-1101
Outpatient Rehabilitation SCI & AMP
Occupational Therapists (OT) in the Outpatient Rehabilitation Service provide service to clients who are 18 years of age and older and reside in Manitoba and Nunavut with specific diagnoses that include:
- Spinal Cord Injury (SCI)
- Complete or incomplete spinal cord injuries
- Acute or long standing
- Central cord syndrome
- Spinal stenosis
- Transverse myelitis
- Spinal cord tumor
- Amputation (AMP)
- Upper or lower extremity amputations
- Acute or long standing
- Clients residing outside of Winnipeg may be seen in consultation with their local primary OT
- Clients residing in Winnipeg may be seen in consultation/collaboration with their community therapist if the client has both community and rehabilitation outpatient therapy needs
- Clients whose goals/issues can be met in an outpatient setting and are not community based
- Clients must have active rehabilitation goal(s)
- Clients need to be medically stable, tolerate sitting up for the time frame needed to attend a one hour or longer appointment and be able to attend and actively participate in appointments at Health Sciences Centre
- Clients who require assistance with personal care will need to bring a support person to assist them with these needs during their appointment
- Clients must understand and agree with the referral to this service
- Referrals will be accepted from health care providers
- No self-referrals accepted
Exclusion criteria
- Clients unable to attend appointments at the Health Sciences Centre
- Clients currently admitted to hospital
- Clients who have issues directly related to fall prevention, management at home or home environments
- Clients who have issues related to homecare care plans, transfers or equipment
- Clients with third party insurance coverage (e.g. MPI, WCB)
- Injuries or diagnoses to hand(s) that are not spinal cord related
- Interventions for diabetic hands (e.g. splinting)
- Clients who are ambulatory and require a wheelchair for long distances or outdoor mobility only
- Clients requiring return to work assessments/interventions
- Clients being paneled or residing in personal care homes
How to refer
Outpatient Rehab AMP and SCI Referral Form
Referral Sources Accepted:
- Primary care providers
- Nurses
- RR2 SCI and AMP clinic
- Allied health professionals
- Prosthetists
- Spinal Cord Injury Manitoba
Referral categories
Referrals that meet our eligibility criteria are assigned a category based on the reasons identified on the referral form. See below list of referral categories and example reasons.
Urgent:
- 24-hour Pressure Management issues – Clients with active new skin issues, transfers contributing to skin issues, pressure injuries from seating system, etc.
- Safety issues – Clients who seating systems pose risk for injury, clients who can no longer operate their mobility base safely, etc.
- SCI Splinting – prevention of contractures, progression of function and time sensitive post Botox
Priority:
- Upper Extremity Amputation Function – Require a rehab program and/or education for compensatory techniques and/or prosthetic training
- Upper Extremity SCI Function – Upper extremity assessment and retraining programs for promotion of upper extremity function (i.e. hand therapy programs, functional electrical stimulation, Saebo splints, etc.)
- Seating, Positioning and Mobility Assessment of clients in temporary rental seating – clients who are in rental seating and/or mobility equipment that require assessment and prescription of a permanent seating system
- 24-hour pressure management issues – clients with chronic skin issues
Standard:
- Seating, Positioning and Mobility Assessment – Assessment and reassessments of permanent seating and mobility systems. Priority is given to clients needing assessment or follow-up for their initial permanent seating/mobility system.
- Wheelchair Skills Assessment and Training – Manual or power wheelchair skills assessment and training.
- Functional Re-Training – Skills-based rehab program intended to optimize function and independence related to functional mobility (i.e. transfers, bed mobility, etc.), self-care/ADL and/or IADL performance
- Follow-up for active rehabilitation goals for clients recently discharge from hospital (examples: completion of permanent seating and mobility goals, increasing functional independence in the area of mobility, transfers, activities of daily living (ADL) and instrumental ADL’s)
What to expect
Screening of Referrals
All referrals are reviewed. Should a referral not meet our eligibility criteria, we will send the referral back to the referral source. If appropriate, we will recommend the appropriate service to refer to.
Initial Assessment: A comprehensive evaluation will occur tailored to the referral issues.
Follow up Assessment and Interventions: Further appointments and interventions will be individually determined and guided by the initial assessment findings. The total number of follow up appointments required and the time frame needed to work through the presenting issues will range depending on the situation.
Consultative and Collaborative Role
Our therapists can provide consultation to clients with a primary OT. Examples include:
- Clients from rural communities – these clients may not be able to come to Health Sciences Centre for assessment/intervention or will require follow-up that would best be completed in the community instead of frequent appointments at HSC
- Clients with significant community/ home environment needs
- Clients with 24-hour pressure management issues that require community occupational therapy intervention related to equipment, home care needs and transfers
Contact information
Occupational Therapy -Outpatient Rehabilitation (Amputations and Spinal Cord Injury)
RR180-800 Sherbrook Street (Pink Goose Zone, Level 1)
Phone: 204-787-8530 for all inquiries about this service
Fax: 204-787-1101 for all referrals
Resources
Renal OT
Renal occupational therapy (OT) provides outpatient services to individuals who are followed by the Manitoba Renal Program interprofessional team at HSC Winnipeg. Clients qualifying for HSC Renal OT services include:
- In-center hemodialysis patients
- Home hemodialysis patients
- Renal health clinic patients
- Local center hemodialysis patients
Renal OT services are provided to clients who require thorough assessment, intervention and follow-up (6-10 sessions). Referrals that can be addressed within 1-4 sessions may be redirected to community organizations that may be better equipped to address episodic care needs.
Referral criteria
Referrals will be screened and may either be accepted or redirected based on renal occupational therapy service criteria.
As renal occupational therapy services address longer term interventions, some referrals that can be addressed within 1-4 sessions may be redirected to community organizations that may be better equipped to address episodic care needs. Redirected referrals are an effort to work collaboratively with community programs and to enhance access to timely therapy services while reducing duplication of services and wait times overall.
Referral Process
Referrals are accepted from healthcare professionals within and outside of HSC. Referring healthcare providers interested in renal OT services must complete the following:
Renal OT Referral Tool — to be completed and faxed.
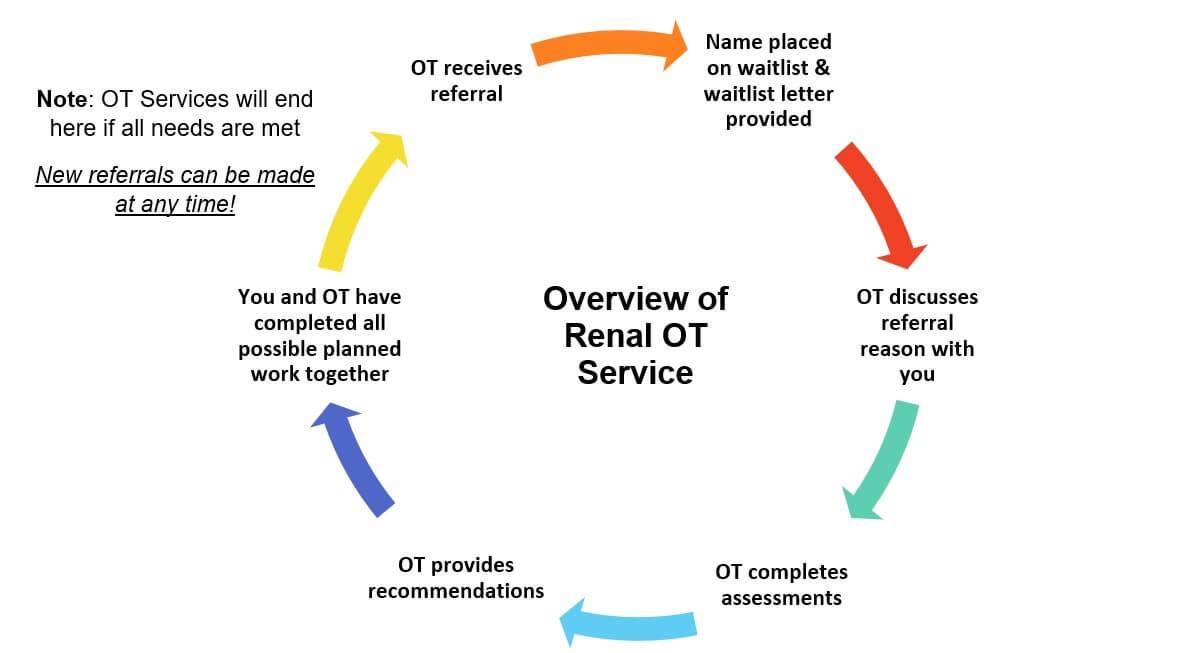
What to expect
Your referral will be screened and if accepted, renal OT will contact you and your family to begin the assessment process.
Renal Occupational Therapy Services can be provided in the following ways:
- During dialysis treatment
- While attending outpatient Renal Health Clinic appointments
- Over the phone
- In the Occupational Therapy Department located in the rehab hospital (RR180)
If your referral is in relation to adaptive or mobility equipment, you and your OT will have a conversation about available funding. You may be expected to pay for some equipment as it may not all be covered through Manitoba Health.
Outlined below are expectations for you and the renal OT:
| Client Expectations | Renal OT Expectations |
| Be an active participant, which means: o Attending all scheduled appointments o Providing information to OT during appointments (funding, insurance, housing layout) o Communicating with OT after appointments (to organize getting your equipment to you) Be clear about goals: o What you need the wheelchair for (long distances, all mobility) Proper use of trial equipment, which means: o Paying for repair or replacement cost of damaged equipment o Giving trial equipment back to OT | Carry-out assessments: o Mat assessment o Skin check o Wheelchair skills Recommend trial equipment: o Discuss features, pros and cons with client Give education about: o Equipment upkeep o Funding availability and guidelines Get equipment from vendors (trial and final equipment prescription). |
Contact information
800 Sherbrook St.
JM519 (Blue Dr. Goodbear Zone, Level 5)
- Phone: 204-787-2786
- All referrals can be faxed to 204-940-2411
Rheumatology
The adult rheumatology outpatient occupational therapy (OT) service focus is on assessment and intervention for clients with upper extremity issues relating to certain chronic health conditions including arthritic and repetitive strain diagnoses.
Referral criteria
- Must have a medical diagnosis of any of the following:
- Osteoarthritis
- Rheumatoid Arthritis
- Lupus Arthritis
- Psoriatic Arthritis
- Scleroderma
- Carpal Tunnel Syndrome
- Cubital Tunnel Syndrome
- De Quervain’s Tenosynovitis
- Trigger Finger
- Referrals must be made by physicians but are accepted from other allied health professionals on a case-by-case basis.
- Client is 16+ years old.
- Clients followed by Child Health outpatient rheumatology OT may be transitioned to adults at 16 years old should the client still require services.
Services provided
- Initial assessment for client and therapist to meet and discuss current issues relating to their diagnosis and participation in daily activities.
- Education regarding health condition(s).
- Client-centered collaboration to help maximize meaningful occupations.
- Custom orthoses/splinting for pain control and/or joint positioning.
- Review and recommendation of assistive devices and equipment.
- Energy Effectiveness education.
- Client advocacy.
- Referral to other community supports as determined.
Referral process
Once a referral is received, it is screened by the OT to ensure the client is eligible for the services. Once the client is accepted, the client is contacted by the office staff of the OT Department, typically by telephone, to book an appointment.
Please fax all referrals to 204-787-1101.
What to expect
The initial appointment with the OT can typically be 60-90 minutes in length for assessment and intervention of presenting issues. When you arrive, please check-in for your appointment at our main office. If you have any existing splints or braces, please bring them with you to the first appointment.
The OT will review the referral information, discuss available options for intervention, and provide those during the appointment after a plan is agreed upon with the client. Follow-up appointments may be scheduled depending on need (may be conducted virtually or in-person).
Contact information
800 Sherbrook Street
RR-180, Pink Goose Zone, Level 1
- Phone number: 204-787-2786
- Fax number: 204-787-1101
Specialized Seating Service (SSS)
We are an outpatient clinic-based service for adults who are experiencing complex seating or mobility-related issues that cannot otherwise be met through primary therapy resources. Referrals are accepted from an individual’s primary therapist only as this service operates consultatively.
Criteria for referrals
Referral requirements for this service include the following:
- Individuals who are 18 years or older
- Use a wheelchair full-time to function
- Have a neurological diagnosis
- Seating or mobility issues are complex and cannot be addressed with primary therapy resources alone
Must have a primary therapist who agrees to remain involved throughout the consultative process.
Referral categories
There are five main categories of referrals:
- Pressure management – for anyone experiencing issues with pressure injuries and/or a history of wounds that are seating-related; includes comprehensive investigation of pressure management behaviours over a 24-hour period
- Posture management – for anyone experiencing issues with how they are positioned and/or receive postural support in their wheelchair; includes issues related to loss of position when sitting
- Functional mobility – for anyone experiencing issues mobilizing their wheelchair (either manual propulsion or power driving); includes wheelchair skills training as well as education and interventions to minimize shoulder injuries
- Assistive technology – for any issues related to driving a power wheelchair using alternative drive controls; includes driving issues combined with any other pressure or postural issue
- Education – formal and informal education opportunities are available for any healthcare providers, funding agencies, and/or consumers experiencing complex seating or mobility related issues
How to submit a referral
Referrals are accepted from individual’s primary therapist only. Therapists who are interested in referring to our service must complete the following:
- SSS Intake and Referral Form – for all referrals regardless of category
- SSS Questionnaire – for all referrals regardless of category; the primary therapist initiating the referral can refer to the SSS Questionnaire Clinical Guide for support materials to help complete this questionnaire when sending in a referral
- SSS Pressure Management Assessment Tool Version 1.0 – for all pressure management referrals
- SSS Re-referral Consult Form – used only in situations where an individual was previously seen through SSS and has been discharged within the last 12 months
What to expect
- Phase 1– Intake and Screening: Upon receipt of a completed referral package, the SSS Intake Coordinator will schedule a virtual Intake/Screening appointment to occur with both the primary therapist and individual being referred where indicated (this appointment will occur within 4-6 weeks of a referral being received). The purpose of this intake appointment is to:
- Confirm and clarify presenting issues
- Determine urgency and waitlist priority of the referral
- Provide interim recommendations for the primary therapist and individual to proceed with while waiting to be seen through SSS
- Phase 2 – Initial Assessment: A comprehensive evaluation will occur tailored to the referring issues (this appointment will occur either in person or virtually depending on each individual scenario and typically lasts 3 hours).
- Phase 3 – Follow-up Assessment and Interventions: Further appointments and interventions will be individually determined and guided by the initial assessment findings. The total number of follow-up appointments required and time frame needed to work through presenting issues will range depending on the situation. Typical follow-up appointments can last between 1-3 hours each in duration and on average 3-5 visits in total will be required to work through this phase. It is common to have gaps in time between appointments whenever trial equipment needs to be sourced from equipment suppliers as part of the intervention strategy. The time frame to work through these follow-up interventions and equipment evaluations typically can last between 2-6 months (or more) depending on the complexity of the situation.
- Phase 4 – Equipment Prescription and Acquisition: Once the intervention/evaluation process is completed the SSS therapist will work collaboratively with the primary therapist to support any justification required to prescribe any recommended equipment. Consultation about how to navigate through the various funding systems for seating and wheeled mobility equipment will be provided on an individualized basis.
- Phase 5 – Fitting and Training: The last phase of the intervention process involves fitting individuals with any equipment that has been prescribed. Education and training with any new equipment is also included in this phase. The time frame to work through fitting is also individually determined but commonly requires 1-4 additional visits. These fitting appointments can last anywhere between 1-6 hours each.
In-person vs. virtual appointments
An individualized plan will be put in place to determine whether each appointment should occur in-person, virtually, or through more indirect consultation to the primary therapist. A number of factors will be considered whenever deciding how each appointment should be carried out.
Whenever in-person appointments occur, it is mandatory for both the individual wheelchair user as well as the primary therapist to attend.
Whenever virtual appointments occur, both the individual wheelchair user and primary therapist are expected to attend at the same remote location. It is also common for interventions to be delegated solely to the primary therapist for follow-up. In these scenarios, the SSS therapist can act more as an indirect consult to that therapist as support is needed to carry out the intervention plans.
Contact information
SSS main location
RR160E-800 Sherbrook Street (Pink Goose Zone, Level 1)
Phone: 204-787-4266 for all inquiries about this service
Fax: 204-787-1101 for all referrals
Seating and Mobility Clinical Specialist
- Phone: 204-787-4266
- Fax: 204-787-1101
Assistive Technology Clinical Service Leader
- Phone: 204-787-2370
- Fax: 204-787-5099
Resources
Information coming soon. Check back often!
Ambulatory Care Services
- Burns and Plastics



