National Healthcare Facilities & Engineering Week 2021
Our Facility Management team is responsible for keeping HSC Winnipeg safe and operational. Our team plays a vital role in addressing comfort and building concerns from every area of Manitoba’s hospital, with our staff and patients being the top priority.
In recognition of National Healthcare Facilities and Engineering Week, we are highlighting different parts of their work. You can learn more below.
Fresh air is key
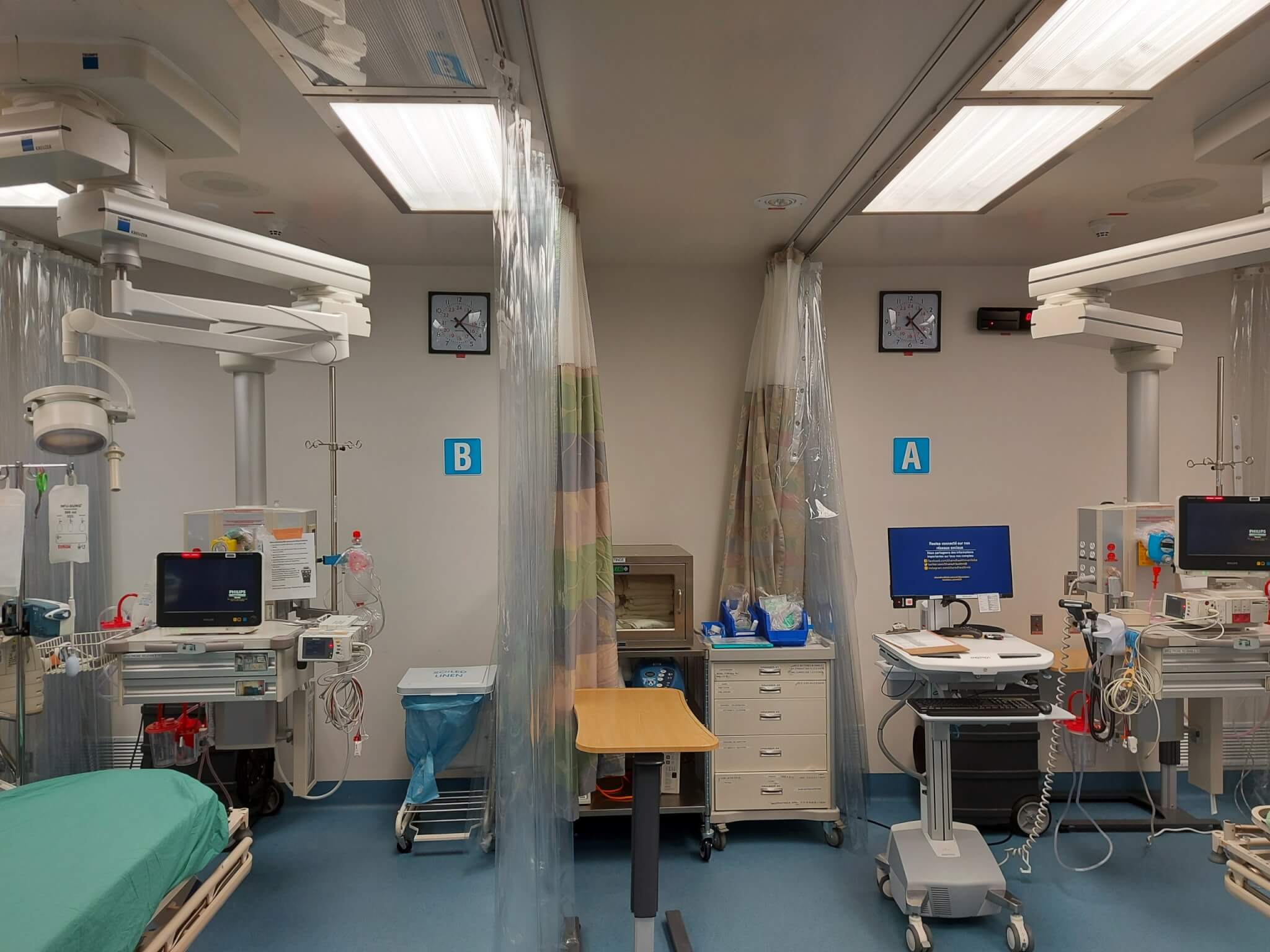
Resuscitation rooms in emergency departments are used to provide urgent care to patients in medical distress. With insufficient time to test the presenting patients, staff risk exposure to infectious diseases during aerosol generating medical procedures. While personal protective equipment such as masks and gloves provide protection, the addition of engineering controls can make the room a safer environment.
- Physical barriers such as non-permeable plastic curtains and glass enclosures around patient beds provide a physical barrier to reduce the spread of droplets and protects patients, staff, and equipment.
- HEPA air filters clean and recycle the air within the resuscitation room. Used in conjunction with plastic curtains, the HEPA room air purifier extracts air from around the patient bed, cleans the air using HEPA air filters, and then returns it to the room. Correct placement of the unit, combined with the building ventilation system, helps induce air flow towards the patient and reduces the migration of airborne droplets around the room.
- Negative Space Pressurization: Airborne droplets produced in resuscitation room can be contained within the room by using negative space pressurization. Increasing the amount of air removed from the space, through increased fan speeds or adding ventilation equipment, will force air to flow from adjacent spaces into the resuscitation rooms and prevent the migration of airborne droplets out of the resuscitation room.
Ultraviolet lights to disinfect
Following a thorough terminal clean, our Housekeeping team uses mobile UV lights to finish disinfecting and sterilizing the operating room theatres and patient care rooms. UV lights are an effective additional cleaning practice against the many germs and viruses that normally exist in a hospital environment.
Heating, cooling, and humidity levels throughout HSC
Our Facility Management, and Operations and Maintenance teams recently completed a large-scale steam trap audit. This maintenance work provides tremendous operational and environmental benefits.
HSC runs on boilers located at the Central Energy Plant. These boilers generate 514 million pounds of steam annually, which is distributed to buildings for heating, hot water, sterilization, and other activities. Steam traps are found throughout steam systems, with approximately 3,500 traps throughout HSC. These steam traps remove condensate and other non-condensable gases while not permitting live steam from being lost. It is natural for any mechanism to suffer wear, and steam traps are no exception. When steam traps fail, energy is wasted and there is possibility for system failure.
Working with Efficiency Manitoba, our teams undertook the large site-wide audit in phases, repairing or replacing all traps that didn’t pass inspection and improving our steam distribution.
The benefits are significant. Repairing deficiencies will save approximately $120,000 per year through reduced steam losses. HSC’s overall CO2 emissions will also be decreased by approximately 950 tons per year. Additionally, the steam trap audit provides valuable systems documentation to O&M. These documents will allow continuous improvements to be made to the steam distribution system for better ongoing energy management saving energy, money, and the environment in the long term.
Calculating air exchange rates and determining air clearance times
We always want our systems to be delivering clean, conditioned air that is suitable for a healthy environment for patients and staff. The COVID-19 pandemic has made us pay particular attention to the prevention of possible outbreaks, and critically examine how HVAC systems function.
A negative pressure isolation room can be used to mitigate the spread of a virus with airborne properties. There are certain situations, however, where isolation rooms can’t be used, such as when they are all being used at the same time and more space is needed, or when patients need to be brought to non-isolation rooms for special procedures.
As more areas of the hospital are being used to treat people with possible contagious illnesses, it becomes necessary to minimize exposure to other patients and staff. Determining when it is safe to bring a new patient into a possibly contaminated room becomes very important.
To calculate the length of time necessary to clear a room of possible airborne contaminants, a couple of variables need to be found. The volume of the room and the amount of air entering or leaving the room needs to be determined. Room volumes can be calculated from direct measurements or obtained from architectural drawings or databases. Airflows can be obtained by measuring or by looking at air balancing reports.
The air exchange rate (air changes per hour) can be obtained using a specific formula. After obtaining the air changes per hour value, our staff review a chart from the Centers for Disease Control and Prevention (CDC) to find the time in minutes required for removal efficiencies of 90%, 99% and 99.9% of airborne contaminants. Once the amount of air clearance time is determined, staff can plan patient flow through various areas of the hospital with a minimized risk of outbreaks due to potentially contaminated room air.
It is quite common to see rooms designed with more supply air than return or exhaust air. This would mean that air naturally wants to leave the room and enter the surrounding area. Sometimes it is possible to rebalance the air so that there is less supply relative to the return or exhaust. This can sometimes be done for a single room or even an entire patient unit. If the airflow into a room cannot be changed then at least a physical barrier like a closed door would help to contain airborne contaminants. The use of proper signage on closed doors help staff understand the potential risks behind the doors and could be used to inform staff of air clearance times.